I was preparing to intubate Kacey* in the COVID-19 intensive care unit when I looked up and saw Americans storming the U.S. Capitol on his television.
"What the hell is going on?" I thought. "Is this real?"
While the nurse was getting intubation drugs, I looked over to my respiratory therapist, a friend and colleague with whom I have worked for several years. "Larry ... look." I nodded up at the television, which showed people crowding the Capitol entrance and some breaking windows. It felt like watching a swarm of angry bees attacking everything in sight. Kacey was on non-invasive ventilation — BiPAP. It is similar to the CPAP masks some people wear for obstructive sleep apnea, but he needed it to keep his oxygen level marginal. He was trying to talk through the BiPAP and kept holding up four fingers as he tried to update me on what was happening, but I could not understand.
"Save your breath," I urged him. This was especially hard. I had become attached — again. But how could you not? He is such a nice guy — charming, funny and used to being in control. He owns his own business — built it from the ground up, he said. Now, he was scared. He had heard all the stories. He knew that being sick enough to need a breathing tube meant he could die. He has a family he loves. He has friends who are like family. I understood.
For the first couple of days, though, he looked good. Each day he asked how I thought he was doing. "You are the healthiest patient I have in the ICU right now," I told him.
A lot can happen in 24 hours.
I frequently tell my kids, "We have the family we are born with, and those we pick up along the way." Kacey clearly ascribed to the same ideas. He had friends coming out of the woodwork to check in on him. He told me the first day we met that he had a close family friend who was a pulmonary/critical-care doctor. Kacey asked me to talk with him.
His friend and I had been in communication for a few days already. I could see why they were friends — I don't think either one of them had ever met a stranger. That afternoon was going to be a painful discussion.
At the moment, he was still holding my hand, as he had been since I told him he was going to need a breathing tube. He was scared, and I was concerned for him.
"It's OK. I'm right here, Kacey. I'm not going anywhere. We're going to take care of you." He squeezed my hand twice in rapid succession. This had become how he communicated "thank you" while air was insufflated into his lungs through the mask on his face.
As I waited for the drugs, I looked up again. The crowd on the television had grown, and someone with a stick or bat was hitting a man who appeared to be a police officer. I looked away as images flooded my mind.
I saw the face of a 99-year-old World War II veteran who had died from COVID earlier that morning. I saw his daughter sitting by his bedside, holding his hand while talking with him. I heard his daughter's voice telling us how her father's military plane had gone down over the Himalayas during a monsoon. He was the only one who walked away. He had survived World War II. He had survived a plane crash. He succumbed to the war on COVID.
I saw the faces of the patient and family I left just moments ago. They were next door, sharing a wall with Kacey's room. Because Henry was dying, he was allowed two family members. His wife and daughter were at his bedside, and several others were on the phone.
Henry had come to the mainland from Hawaii in his early twenties, looking for new opportunities, a new life. He met his wife at church in Chicago. He became a graphic artist, and after he retired, he taught art to children. We had reached this point several times already. His daughter raced to the hospital one night because we thought we were going to lose him. This time, we were.
As I left the room, a small voice came over the phone: "I love you, Grandpa." I bit the inside of my lip and left the room, closing the sliding glass door behind me.
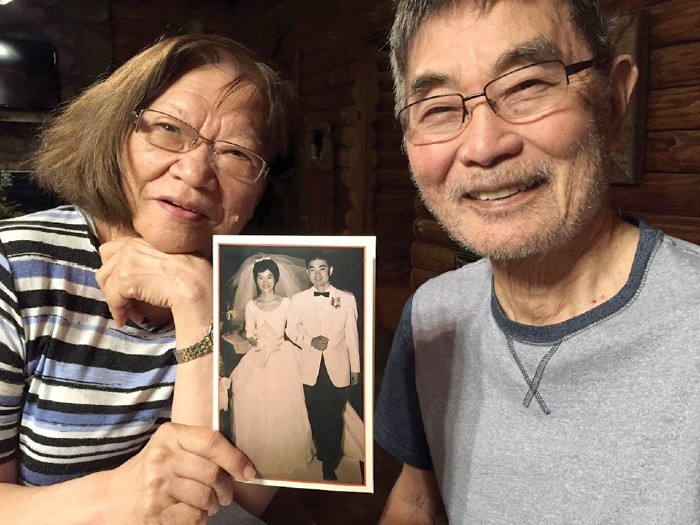
Henry was not going to make it to his 60th wedding anniversary, just a few months away — he was going to die in the same month that my World War II patient would have turned 100 years old. For some reason, all this made what I was seeing on the television seem even more wrong.
"Dr. Osborn, what doses do you want?"
I turned to the resident. "Ian, what do you think?" I work at a teaching facility, and the next generation must learn. We made the decisions on the drugs and proceeded to put Kacey to sleep and temporarily paralyze him. I watched on the monitor as Ian skillfully moved the tongue out of the way. We could see part of the vocal cords. I pressed down on the thyroid cartilage and moved it slightly to the left for him.
Now we could fully see the cords — the gateway to the trachea. We quickly completed the intubation, and Larry began the process of securing the breathing tube and connecting the ventilator.
I looked up at the TV screen again. Someone appeared to be hitting another person with a pole that was flying the American flag. Here we were, hooking Kacey up to a machine that would provide more effective breaths for him while I was watching something that took away mine.
Then I closed my eyes and saw the face of my husband on the day he was mobilized to Afghanistan as an Army Special Forces officer. He was smiling and trying to dance with his eight-months-pregnant wife while Bob Marley's song "Three Little Birds" played in the background. A few days before, he had gone through the paperwork and administrative details I needed to know while he was overseas.
"This file has all the bank account information. Here is the power of attorney. Oh, this is the folder with information if I need a flag."
"What do you mean if you need a flag?"
"This organization provides the flag for the coffin." He met my eyes and tried to smile reassuringly. "If it is needed."
I just stared at him. "Really?" I thought. "Did you really have to tell your eight-months-pregnant wife about the coffin-flag folder?" I understood him. Organization and preparation is how he cared for me as we faced him leaving. Still, it was a completely guy thing to do. So smart and yet so not. I had several choice thoughts for him — which I said quite eloquently in my mind. Of course, when I opened my mouth, all that came out were sobs weighed down with the fear that he might not come home. Through crumpled, soggy tissues, I told him our discussion on that topic was over.

After that, it was not hard to get him to make the two videos before he left. One was of him reading three children's books as if he were reading them to Ashley, after she was born. I figured if we "read books with Daddy" by video, maybe he would not seem strange to her when he returned. The second video was a message from him to her. Something I could give her when she was old enough if he did not come home.
After he was gone, I would double check all the doors at night to make sure the house was locked. That had been his job. For some reason, it never felt as safe when I did it.
More unsettling was waking up each morning wondering if that would be the day someone would pull into my driveway to tell me he was not coming home.
In the ICU, I looked up again at the mob on the TV. We made sacrifices for our country — not for this. I bit my lip again.
"Great job, everyone. His oxygen saturation looks good. We will see how he does over the next couple of hours. We will have a low threshold to prone him." Had my voice cracked? Had anyone noticed?
When I left the room, tears welled. Luckily, people cannot really see much when you are wearing goggles, a face shield and a mask, but I knew I needed to find a private space. It happens like that sometimes. When the focus required to get the job done is no longer required, the emotions poke their heads around the corner and climb over all the walls you put up to complete the task.
There is one bathroom in the ICU, and it is about the size of Barbie's closet, so not very popular. I locked the door and hung my goggles and face shield on the door's coat hangers, next to a pair of goggles that had been there for a few days. Quietly, carefully, I let myself cry.
Now I saw the face of Uncle Olan. He served in World War II as one of Carlson's Raiders, the precursor to today's Special Forces. He was smiling at me. I never really registered the facial deformities from his injuries that my family discussed. Maybe the surgeries were just that good, or maybe I saw him through the eyes of a child who loved him. I saw the beloved uncle in the bathrobe who raised an eyebrow, watching me struggle with our games of candy poker or candy blackjack in his room at the VA.
He made sacrifices for his country — not for this.
I thought of my grandfather and the World War II injury that marred his voice and caused him to speak in a cadence that was sometimes difficult to understand. I thought of my sister-in-law, who served the military legal system her entire career, and her parents, who also served our country.
The Korean War Memorial says it simply: "Freedom is not free." Those sacrifices were not made for the freedom to invade the nation's Capitol.
Many things are contributing to what is happening in our country, but what I thought about that day was misinformation — conception and propagation. Both the manipulators and the manipulated should be held accountable for their actions.
I was angry, sad, disappointed and scared. As I wiped away tears in the Barbie-closet bathroom, I realized what happened that day does not represent the America I know. We are not defined by what occurred. We are defined by how we respond. Although it feels dark, light emanates from truth. It emanates from kindness, from courage, from caring for one another. Those are the threads of light woven through the fabric of the American culture I know.
"I understand this is not enough," I thought, "but it is enough to start." I put on my N95 and grabbed my goggles and face shield off the door hook.
I needed to check in on bed 5. She is so friendly and full of life. She would invite the janitor to dinner if he was not moving too fast down the hall in front of her room. Every day she asks, "Am I going to be okay, Doc?" The day prior I started telling her, "You are the healthiest person in my unit right now."
"Dr. Osborn!" The nurse caught me as I was walking out of the Barbie-closet bathroom.
"Yes?"
"Henry just died. The resident is in another room, and someone needs to pronounce him."
"Thank you. I'll take care of him," I said, and walked toward his room.
*Most patient names were changed to protect privacy. Patient families gave permission/signed HIPAA permission forms for their stories to be used in this essay.
Dr. Tiffany Osborn is professor of surgery and of emergency medicine at Washington University School of Medicine who works in the intensive care unit and emergency department. She is the Physician Champion for BJC HealthCare Sepsis Quality Improvement. She co-directs the COVID Critical Care Committee, the Convalescent Plasma Program, and Contingency and Crisis Standard of Care at Barnes-Jewish Hospital.
Dr. Osborn has been featured on NPR and CNN, as well in radio interviews and local media. She'd like to thank Jeannette Cooperman and Judy Martin Finch for their thoughtful review.